Immune Cell Redirecting Therapies
Novel method sheds light on developing therapeutic against B cell cancers and facilitating rapid drug discovery
Leukemia is the most common cancer in children, accounting for almost one out of three cancers. Children’s Healthcare of Atlanta, an Emory University partner, sees over 150 blood cancer patients each year alone.
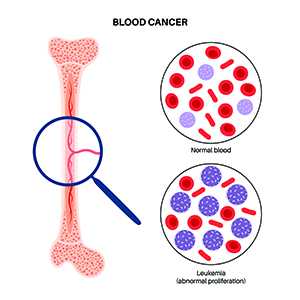
The most common type of cancer in children is acute lymphoblastic leukemia (ALL), an aggressive blood cancer that starts in the white blood cells of the bone marrow. Typically, ALL affects the B and T cells in the immune system, with B cell ALL (B-ALL) affecting mostly children. Traditional treatments for leukemia, like chemotherapy or radiation therapy, can have significant side effects on patients such as hair loss and organ damage.
However, one promising leukemia treatment – immune cell redirection (ICR) – is emerging thanks to Emory researchers. ICR is a powerful and versatile therapeutic approach that redirects the anti-cancer T cells to target cancer cells via drug-induced cell binding.
A promising therapeutic for B cell leukemia
Erik Dreaden, PhD, is a pioneer in using molecular engineering to improve cancer immunotherapies. Now, the assistant professor at Emory’s Department of Pediatrics and Biomedical Engineering leads the development of an ICR therapy to target B cell type cancer.
Named bispecific T cell-engaging cytokines (BiTEokines), this particular chemical architecture designed by Dreaden and his lab delivers and screens for ICR drug candidates, yielding multiple therapeutic functions. BiTEokines can activate and redirect the lytic ability (the ability to break down cells) of the enriched subsets of T cells in leukemia patients toward the cancerous B cells. At the same time, it can co-deliver IL-12, a T cell-stimulating cytokine, to enhance the proliferation and lytic activity of the T cells.

Erik Dreaden
“What's interesting about the therapeutic effects we observe in leukemia mouse models is that this approach provides prophylactic protection against cancer,” said Dreaden. “Think about it like a vaccine response in the sense that the patients can generate immune memory to prevent relapse at a later date.”
The ability of this therapeutic to confer antileukemic immune memory is a promising step in resolving the relatively short relapse-free time of B-ALL. This can be seen in other leukemia treatments such as blinatumomab, an FDA-approved ICR drug that links anti-cancer T cells and cancerous B cells.
“One challenge for patients who undergo immunotherapies is the loss or downregulation of the target antigen presented on the cancerous B cells,” said Dreaden.
This cell repression or loss can be problematic since the cancer cells can escape detection and destruction as T cells lose their target. However, Dreaden and his team have found it’s possible to “park” multiple ligands on the surface of the BiTEokine particles to target more than one antigen on the cancer cell surface for recognition.
A novel way to accelerate the drug discovery process
Traditional techniques for discovering ICR drug candidates are often time-intensive and low-throughput. But Dreaden and his team have come up with a potential solution: a novel method for the assembly of diverse libraries of BiTEokines and their high-throughput screening to identify effective anti-leukemic particles.
“Another parallel application we’ve been exploring for this technology is its potential for rapid assembly and screening of therapies for leukemia and other cancers,” said Dreaden.
In the paper describing this method, the researchers synthesized a library of 46 BiTEokine test compounds, with some found to exhibit lytic activity comparable to current FDA-approved therapies for leukemia. Using this approach, it’s possible to list several potential drug candidates and screen for their effectiveness over the course of days, rather than months using the traditional techniques.
Rethinking future cancer treatment
Speaking of his inspiration and passion for cancer immunotherapies, Dreaden said, “The way we can co-opt the immune system to eliminate cancers without the systemic damage from traditional treatments is very exciting. Some patients can even achieve lifelong complete responses – the absence of detectable cancers – while some patients with advanced diseases can exhibit more favorable prognosis.”
Emory Office of Technology Transfer licensing associate Shweta Ghai, PhD, who works closely with Dreaden, had similar aspirations for the technology.
“This new invention presents a targeted cytokine therapy (IL-12 therapy) or drug delivery vehicle for treating B cell acute lymphoblastic leukemia (B-ALL) with reduced IL-12 off-target toxicity and improved patient response, which could potentially be a savior even for B-ALL patients who relapse when given other existing immunotherapies.”
For future work, Dreaden will continue exploring this invention's application in treating B cell leukemia. Given the compounds' modular nature and rapid assembly, he hopes this therapeutic approach will extend to a wide range of immune cells and other autoimmune diseases.
Techid: 20153
Read our technology brief